Inflammation has become a hot topic in health discussions, and for good reason. While acute inflammation is a necessary part of the body’s healing process, chronic, low-grade inflammation that persists throughout the body has been linked to a wide range of chronic diseases, including heart disease, diabetes, arthritis, and even some types of cancer. What might surprise you is that the health of your mouth, particularly the presence of gum disease, can be a significant contributor to this systemic inflammatory burden. Let’s explore the connection between oral health and systemic inflammation and how oral probiotics might offer a potential way to help tame those internal flames.
Table of Contents
The Oral Cavity: A Source of Systemic Inflammation
As we’ve discussed in other parts of this guide, your mouth is home to a complex community of bacteria. When the balance of this oral microbiome tips towards the less friendly side, it can lead to chronic inflammatory conditions like gingivitis and periodontitis. Unlike a localized infection that your body can usually clear up relatively quickly, chronic gum disease involves ongoing inflammation in the oral tissues. This persistent inflammation doesn’t always stay confined to your mouth.
The Inflammatory Cascade: From Mouth to Body
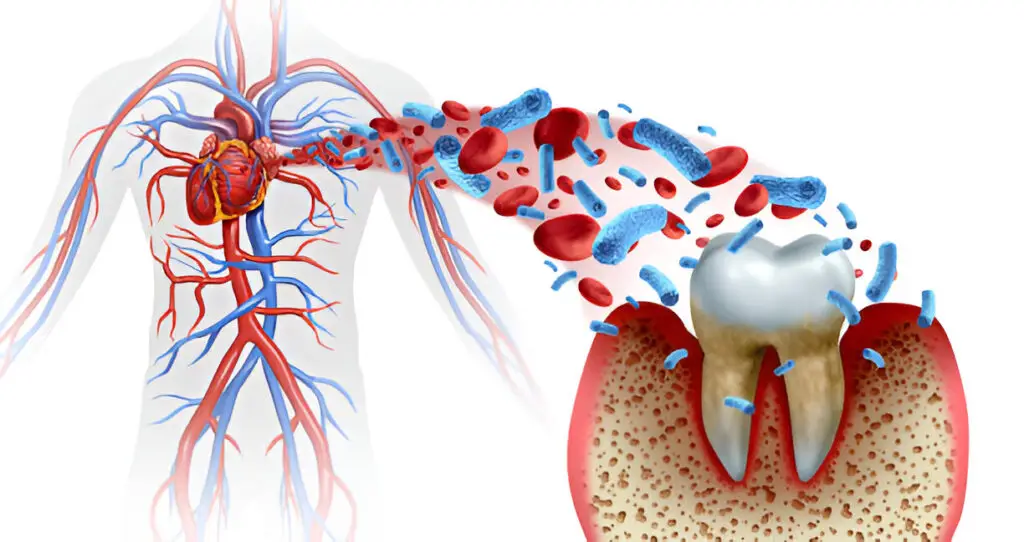
The inflamed gums in periodontal disease create an environment where bacteria and their byproducts can easily enter the bloodstream. Once in circulation, these inflammatory agents can travel to other parts of your body, triggering or exacerbating inflammation in distant organs and tissues. This systemic inflammation is thought to be a key driver in the development and progression of many chronic diseases.
External Link Suggestion: Harvard Health Publishing – Inflammation: A unifying theory of disease
Think of it like a small, smoldering fire in your mouth that can send smoke signals – inflammatory molecules – throughout your entire body, potentially contributing to a larger, more widespread inflammatory state.
Gum Disease and the Risk of Chronic Illnesses
The link between gum disease and systemic inflammation helps to explain why poor oral health has been associated with an increased risk of various chronic conditions, including:
- Cardiovascular Disease: As we discussed in sub-silo 6.3, the inflammation originating in the mouth can contribute to the development of atherosclerosis.
- Diabetes: Chronic inflammation can interfere with insulin sensitivity, potentially making it harder for the body to regulate blood sugar levels. You can find more information about diabetes and inflammation from the American Diabetes Association (ADA).
- Rheumatoid Arthritis: Some research suggests a link between gum disease and an increased risk and severity of rheumatoid arthritis, an autoimmune inflammatory disease. The Arthritis Foundation provides resources on this condition.
- Adverse Pregnancy Outcomes: Inflammation has also been implicated in adverse pregnancy outcomes, such as preterm birth and low birth weight, and some studies have explored a link with gum disease.
Oral Probiotics: A Potential Way to Reduce the Fire?
This is where oral probiotics offer a promising avenue for potentially reducing systemic inflammation by addressing the inflammation at its source in the mouth. By introducing beneficial bacteria into the oral cavity, oral probiotics aim to restore a healthier balance to the oral microbiome and reduce the overgrowth of the harmful bacteria that drive gum inflammation.
Prodentim is formulated with a selection of probiotic strains that are intended to support a healthy oral environment. By promoting a balanced oral microbiome, Prodentim may help to reduce oral inflammation, which in turn could have a positive impact on the overall inflammatory burden in the body.
Learn More About How Prodentim Supports a Healthy Oral Microbiome »
What the Science Says: Research on Oral Probiotics and Inflammation
Research has shown that certain strains of oral probiotics can indeed help to reduce inflammation in the gums. By crowding out the inflammatory bacteria and promoting a healthier microbial balance, these beneficial bacteria can help to calm the inflammatory response in the oral tissues. While more research is needed to fully understand the extent to which oral probiotics can directly impact systemic inflammation, the evidence supporting their role in reducing oral inflammation is growing.
Practical Steps: Taming Inflammation Starts in Your Mouth
Taking steps to improve your oral health is a proactive way to potentially reduce systemic inflammation. Here’s what you can do:
- Practice Diligent Oral Hygiene: Brush thoroughly twice a day and floss daily to remove plaque and prevent gum disease.
- Consider Oral Probiotics: Incorporating oral probiotics into your routine might help to foster a healthier oral microbiome and reduce inflammation.
- Don’t Ignore Gum Issues: If you notice any signs of gum disease, seek professional dental care promptly.
- Maintain a Healthy Lifestyle: A balanced diet, regular exercise, and avoiding smoking can also help to reduce overall inflammation in the body.
Resource: National Institute of Dental and Craniofacial Research (NIDCR) – Periodontal (Gum) Disease
The Future of Inflammation Research: A Holistic Approach
The understanding of the link between oral health and systemic inflammation highlights the importance of taking a holistic approach to health. Addressing inflammation at its various sources, including in the mouth, could be a key strategy for preventing and managing a wide range of chronic diseases. As research continues to uncover the intricate connections within our bodies, oral probiotics may become an increasingly recognized tool in our arsenal for taming the flames of systemic inflammation and promoting long-term health and well-being.